The healing properties of light are wide-ranging; simply getting enough sunlight can improve mood disorders like seasonal affective disorder (SAD), for example. Light therapies are effective at treating skin complaints like psoriasis, acne, or eczema, psychiatric disorders, as well as sleep disorders and improving circadian rhythm.
Photodynamic therapy (PDT) is a more targeted therapy. It uses a photosensitiser, a compound that, upon illumination at a specific wavelength, generates reactive oxygen species that kills cells. In the treatment of cancer, a photosensitiser binding to malignant cells can destroy them when activated by light. Microbial cells are another target for treatment with PDT and the technique is used in dentistry and dermatology – for killing the bacteria causing acne, for instance.
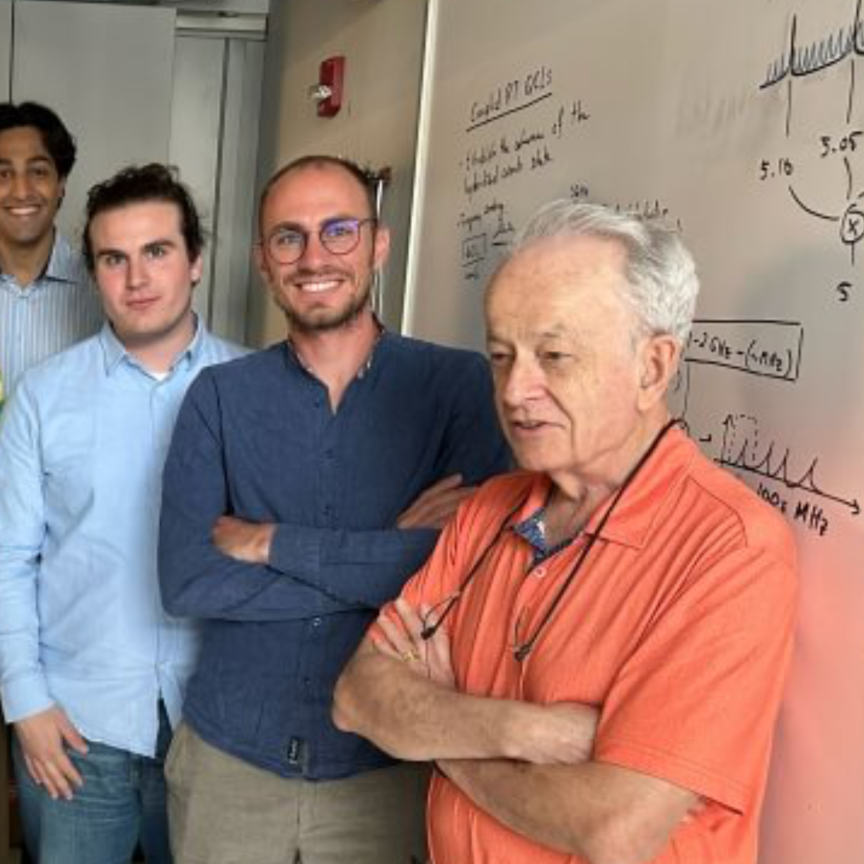
According to Dr Michael Hamblin, of the Wellman Center for Photomedicine, Massachusetts General Hospital, there are clinical trials ongoing for treating various infections with PDT and there are other infections that could potentially be treated with the technique, including drug-resistant bacteria.
‘A lot of people are interested in multi-drug resistant bacteria, which are usually caught in hospitals,’ he says. He says post-surgical infections like MRSA (methicillin-resistant staphylococcus aureus) or dental infections are good targets for PDT.
Dr Hamblin’s laboratory at the Wellman Center for Photomedicine specialises in designing selective photosensitisers for different microbial cells. A lot of his work revolves around studying PDT in vivo in animal models and using bioluminescence to monitor the progress of an infection and the efficacy of PDT at fighting it.
PDT could potentially treat various forms of multi-drug resistant strains of bacteria, such as those for tuberculosis, although Dr Hamblin says TB is challenging because it multiplies internally. ‘The only treatment at the moment for a granuloma from an extensively drug-resistant strain of TB is surgical removal of the lesion. It doesn’t respond to any drugs at all. If that becomes common, then you could envisage treating these granulomas with PDT.
‘With fibre optics, it is conceivable to treat internal infections with PDT. You can thread fibres pretty much anywhere in the body, even to the heart,’ he says. Bacterial endocarditis, for example, an infection of the heart valves with a mortality rate of more than 50 per cent, has been considered for PDT treatment.
Treating birthmarks
At the University of California, Irvine, research is underway to treat port-wine stain birthmarks with PDT. The researchers are in the process of applying to the FDA and the Institutional Review Board (IRB) to conduct clinical trials for treating these vascular malformations using NPe6, a photosensitiser responding to 664nm light, in combination with pulsed dye laser therapy. A port-wine stain is a birthmark whereby extra and often dilated blood vessels create a red or purplish discolouration of the skin. Standard treatment typically involves illuminating the region with a pulse of laser radiation lasting around 1.5ms at 585-595nm, which is absorbed by haemoglobin and can photocoagulate the blood vessels. The treatment method has varying success, with only around 20 per cent of port-wine stain lesions being blanched completely using pulsed dye laser therapy.
The studies at University of California, Irvine, involve augmenting pulsed dye laser therapy with PDT, running a course of PDT to attack the blood vessels and then immediately following up with pulsed dye laser therapy.
‘Pulsed dye laser therapy improves vascular shutdown after PDT,’ says Dr Kristen Kelly, associate professor of dermatology and surgery at University of California, Irvine. ‘Our theory is that PDT causes an initial injury to the blood vessels; by combining this with pulsed dye laser therapy we improve the vessel shutdown, while also providing safer vessel shutdown.’ Dr Kelly is co-principal investigator on the project along with Dr Bernard Choi.
Dr Kelly says that PDT has advantages, in that it can remove blood vessels of all sizes and can treat patients of all skin types, but the danger is that it could remove too many vessels. ‘We use lower doses of light for the PDT, so as to just get the process started, and then follow up with the pulsed dye laser in an effort to achieve better results than would be possible with either treatment alone, and improving safety.’
Dr Kelly says that the precise mechanism for the combined therapy is unknown, but the theory is PDT damages and perhaps dilates the blood vessels. The larger vasculature then provides a better target for the pulsed dye laser therapy. In addition, since PDT has already caused some damage to the vessel walls, further damage occurs when haemoglobin absorbs laser light.
Pulsed dye laser therapy on its own isn’t as effective in darker skin types, as the light has to pass through melanin. ‘If we can use lower-pulsed laser energies because we’ve already caused some damage to the vessels with PDT, our hope is that we’ll get a better result,’ says Dr Kelly.
Port-wine stain lesions can require many, up to 20, treatments, says Dr Kelly. ‘We can lighten the stains with a pulsed dye laser, but it does take a lot of treatments and often we’re not able to remove them completely. In addition to that, even after all those treatments, slowly a portion of the port-wine stain tends to come back over time and people will often require maintenance treatment.’
A course of pulsed dye laser therapy would generally last years, but the hope is that supplementing this with PDT will improve the success rate of the treatment.
Drug delivery
Photosensitisers for cancer treatment aren’t only a direct means to attack cells, but can also facilitate drug delivery. A photodynamic technique called photochemical internalisation (PCI), invented at the Norwegian Radium hospital in Oslo, helps drugs reach their targets within cells by releasing them from intracellular organelles called endosomes.
Cells ingest molecules by a process called endocytosis, in which sections of the membrane engulf molecules from the surroundings before invaginating to form endosomes inside the cell. A lot of molecules, including drugs, remain locked in these endosomes and aren’t released. Thus, a number of drugs have problems passing the cell membrane or get trapped in endosomes and are eventually broken down by enzymes before they can reach their target inside the cell.
Norwegian oncology drug company, PCI Biotech, has developed a photosensitiser called Amphinex, which is specifically designed to adhere to cell membranes. It gets taken up in endosomes along with the drug and, when activated by red light at 652nm, breaks open the endosome thus releasing the contents, including the drug, into the cell. ‘We can use this technology to release those drugs specifically taken up by endocytosis in a specific area of tissue,’ explains Dr Per Walday, CEO of PCI Biotech. The company uses a laser system platform from Modulight, a laser manufacturer based in Tampere, Finland. ‘The photosensitisers are activated by very specific wavelengths of light – they have a defined absorption spectrum so we needed a laser that’s reliably illuminating in that absorption spectrum all the time,’ says Dr Walday.
Modulight’s laser was designed with several channels that can be calibrated independently to allow a surgeon to illuminate different areas at the same time. The channels also provide different energy outputs, so a tumour can be illuminated from the inside and outside simultaneously and still remain effective.
Dr Walday adds that the laser has to be reliable. He explains the process: ‘Patients receive a dose of Amphinex. We then wait a few days, treat with the drug, and illuminate the tumour. We have to illuminate within a certain time window. When you’ve got implant tubes in a patient, if the laser doesn’t work, then you’re in trouble. We need to have a really reliable instrument.’
PCI Biotech is currently running a phase II clinical study using the technique on head and neck cancers, which are typically difficult to treat. Head and neck cancers tend to metastasise very late and a number of patients die from the cancer without it spreading at all.
‘These patients are often treated with surgery and radiation therapy, but when you’ve done that and the treatment hasn’t worked, it’s very difficult to repeat,’ says Dr Walday. ‘At this point, we can come in with this technology and treat those patients that have no other treatment options. We can potentially remove the tumour or at least prolong the patient’s life using PCI; that’s what we’re hoping for.’
PCI has been shown to enhance the effect of a number of drugs already on the market that end up in endosomes. The trial on head and neck cancer aims to enhance bleomycin, a chemotherapy agent on the market, which seems to be taken up to a large extent in endosomes. PCI Biotech has also shown in pre-clinical experiments in animals that Amphinex can enhance the effect of gemcitabine, a relatively modern drug used to treat bile duct cancer. PCI Biotech will be running a study in the spring on bile duct cancer.
Amphinex was designed to be activated by red light at 652nm, explains Dr Walday, as at this wavelength the light penetrates much deeper into tissue than blue or green light. However, 652nm still has enough energy to activate the photosensitiser.
‘This technology can be used for a number of different cancers and for a number of different drugs, even drugs already on the market,’ comments Dr Walday.
‘In addition, if you really design a drug that doesn’t work without PCI technology, then you can have a very specific therapeutic effect upon illumination.’
Developing a photosensitiser for photodynamic therapy (PDT) is an expensive and time-consuming prospect. Researchers at the Wellman Center for Photomedicine, Massachusetts General Hospital have been investigating irradiating microbes with blue light (405nm or 470nm) as a simple alternative to using PDT to combat infections.
‘It transpires that blue light on its own without any photosensitiser is surprisingly efficient at killing pathogens – it’s way more effective than we thought it was going to be,’ says Dr Michael Hamblin at the centre. ‘It’s entirely possible that blue light therapy could supplant PDT, because it’s kind of the same thing in the terms of getting the light to the infected area, but without having to worry about photosensitisers.’
The Wellman Center worked with Helicobacter pylori in the stomach several years ago, which was found to be exceptionally sensitive to blue light. ‘We’ve now found that all sorts of pathogens are actually surprisingly sensitive to blue light – pseudomonas, MRSA; all sorts of things,’ Dr Hamblin says.
‘People are worried with using UV in terms of host tissue damage. It might be difficult to get regulatory approval for germicidal ultraviolet as a therapy for infectious diseases. But blue light has a much more favourable selectivity profile; it’s almost impossible to damage mammalian tissue with blue light, but the bacteria seem to die when exposed to it.’