The inroads being made by photonics into a range of novel biomedical applications are plain to see in market forecasts and research publications; but in ophthalmology clinics the impact is already more concrete.
Optical coherence tomography (OCT) gave lasers a first foothold in ophthalmology in the early 1990s, not just for its ability to provide images of the retina, but also thanks to its neat fit within the culture and work-flows of treatment centres. Ever since, photonics has been exploited in increasingly ingenious ways for both the diagnosis and treatment of eye diseases.
Some of the most striking examples can be found in ocular surgery, where the delicate finesse of a modern laser can replace or augment the surgeon’s scalpel, sometimes allowing entirely new and more effective procedures to be employed.
Cataract surgery is a case in point. The impact of ultrafast laser sources in this sector has been dramatic, creating a market on course to be worth $2.4 billion by 2019, up from $572 million in 2012. Such numbers stem largely from an ageing population, which is increasing the number of potential patients just as new laser-based surgery platforms become accepted.
It is not hard to appreciate the market drivers at work. Historians believe that procedures to treat cataracts in the human eye were first carried out centuries ago, when methods for penetrating into the eyeball and pushing a clouded lens out of its natural position were queasily unsubtle.
The contrast with today’s sophisticated cataract surgeries could hardly be greater. Removing a cataract now means softening the afflicted lens into a soft and malleable form, in a process called phacoemulsification. The broken-up lens can then be sucked or flushed out of the eye, before a pristine synthetic intraocular lens (IOL) is put into position.
This procedure requires the insertion of a small ultrasonic probe to take care of the emulsification, which in turn means first making an initial incision into the membrane (or ‘capsule’) surrounding the lens – a step to be taken with the utmost care, since the new IOL will need to sit within it. Damage to the capsule is highly undesirable, and is known to affect the long-term visual outcome.
Femtosecond lasers offer surgeons the means to make this crucial first cut with much finer control than any blade can offer, limiting the risk of unwanted damage as well as allowing the incision to be made in patterns or spirals, easing entry into the capsule even further.
The scale of the business opportunity now opening up in cataract surgery has attracted several laser manufacturers and some subtly distinct implementations, each now at different stages of their international regulatory process. But a common thread is to further leverage the advantages of ultrafast sources once they have become established in cataract procedures, and apply them in other ophthalmology procedures too.
One example is the Victus platform, originally developed by a joint venture of Bausch and Lomb and ophthalmology laser specialists Technolas PV, which has now been brought entirely under the B+L umbrella. From the start, Victus was envisaged as a single-platform femtosecond laser system capable of supporting not just cataract-related procedures, but also refractive and therapeutic operations too.
To this end, Victus incorporates a swept-source OCT live-imaging system, built into the platform. With it, the operating surgeon can visualise both the locations where he intends to cut and accurately program the depth of incision to be made. In tandem with suitable operating software, the system can even provide auto-recognition of key landmark structures in the eye, and give the surgeon a reliable view of the delicate tissues being operated on.
Photocoagulation: staunching the flow
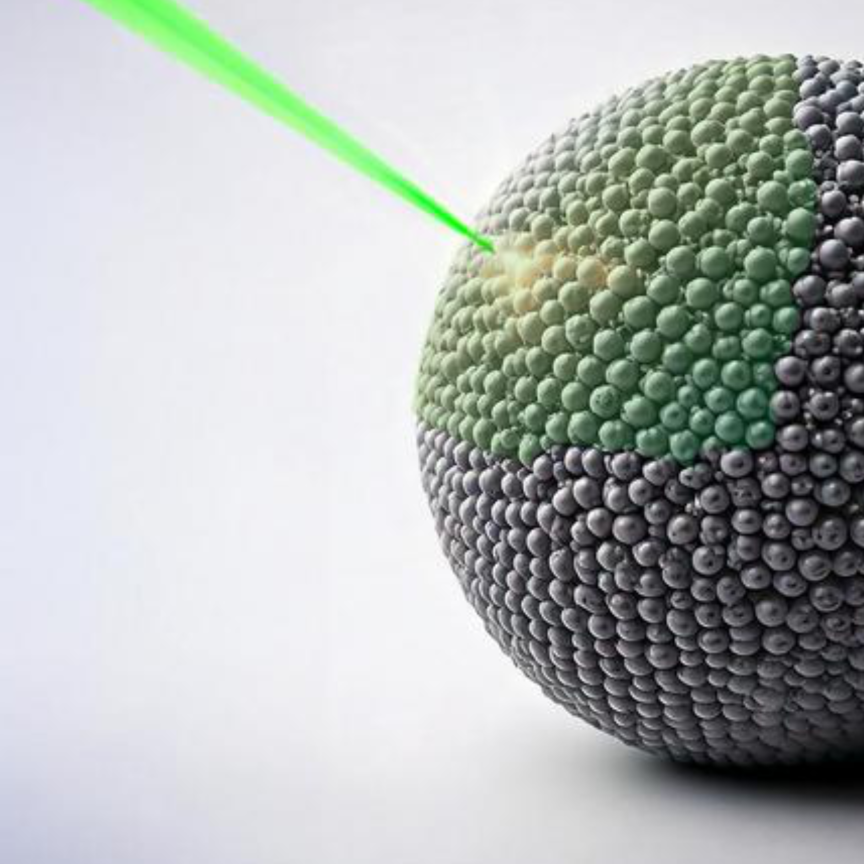
Several eye diseases, diabetic retinopathy and macular edemas among them, feature the presence of leaking or abnormal blood vessels in the retina. Carefully closing these vessels and sealing them shut is an effective way to halt the progress of the disease.
Laser photocoagulation is an appealing tool for this job, exploiting the ability of precisely applied laser light to cauterise the tiny retinal blood vessels – as long as the surgeon has a deft touch. The haemorrhaging must be staunched carefully, or the patient is potentially at risk of discomfort or worse.
Advances in laser technology have already helped to make photocoagulation more precise, but a new platform developed by Quantel Medical has taken a significant further step by adopting both a new emission wavelength and a multi-spot delivery regime.
‘Several laser wavelengths have been used for photocoagulation in the past,’ commented Alexandre Biasi of Quantel. ‘A green emission has been the most common, although a red wavelength can be of benefit when there is some blood present in the eye. But for the Supra Scan 577 system we have employed a yellow source, at 577nm.’
This yellow emission sits close to the peak absorption wavelength of oxyhaemoglobin in the targeted blood vessels, but offers very little absorption by the xanthophyll pigments present in the macula, an oval-shaped pigmented area near the centre of the retina.
In practice this makes the treatment safer to use in locations close to the macula, and means that the surrounding tissues are less affected by heat generated during photocoagulation. The result is a potentially less troublesome time for the patient, as well as a more effective procedure.
‘With other wavelengths, as much as 20 per cent of the energy can be absorbed by the xanthophyll pigment and other substances in the retina, which leads to unwanted degradation of the tissues and makes the procedure more painful,’ commented Biasi. ‘But 577nm is right on the maximum absorption point of the oxyhaemoglobin that you really want to reach.’
The Quantel system also applies its laser light in pulses in the microsecond regime, and does so in customisable multispot patterns rather than single localised spots. This operational combination turns out to have some far reaching advantages, since it reduces the effective exposure time for each individual point under the laser’s gaze while allowing the tolerable power level to be increased.
In effect, a single session with a multi-spot laser can accomplish what would otherwise need multiple sessions with a single-spot source.
According to the company’s clinical trials, reducing the laser pulse lengths from a nominal 100ms to something closer to ten or 20ms allows the laser’s power to be raised from 200mW to around 600mW – although in practice clinicians need to monitor the situation closely, carefully increasing the power levels until the optimum level for an individual patient is reached.
The Supra Scan system also takes advantage of an all-fibre-laser architecture, being built on Quantel’s recently announced Elba platform. This uses proprietary methods to control pulse duration without affecting the power levels of the individual pulses, countering a possible problem in systems which use a galvo mirror to scan the source spot across the fibre and control pulse duration by that method. Instead, the Quantel technique keeps each pulse precisely centred in the fibre, ensuring that spot-to-spot consistency stays at a high level.
Elba could also find use in other clinical applications, thanks to the variety of wavelengths it is designed to deliver in the near-IR and visible ranges. DNA sequencing equipment could be one particularly successful niche, not least thanks to the compact size of the platform and the inherent advantages of a fibre laser design.
Retinal implants: restoring what was lost
In July, a partially sighted British pensioner made headlines worldwide after having his central vision restored thanks to a retinal implant manufactured by US-based company Second Sight.
Ray Flynn, 80, suffered from age-related macular degeneration (AMD). His impaired sight was one individual’s experience of a significant global health challenge, as an ageing population encounters a number of potentially serious retinal diseases.
In Flynn’s case, the solution came in the form of Second Sight’s Argus II system, in which a miniature video camera, housed in glasses and worn by the patient, captures image information which is processed and transmitted wirelessly to the implant surgically positioned in the retina.
An antenna in the implant picks up the signal, and an electrode array duly emits small pulses of electricity to the retina’s remaining functional cells for transmission to the optic nerve and the brain - an architecture which bypasses the failed photoreceptors damaged by the disease. The patient duly perceives patterns of light, and learns to interpret these as visual patterns.
Second Sight has been developing retinal prostheses since its founding in 1998, and recognises that the technology has come a long way since then.
‘We created the first Argus I system in 2002, and it took ten years to make Argus II,’ commented Second Sight’s Gregoire Cosendai. ‘With Argus II we have a minimally invasive wireless system, which is critical. Stability and safety are the key objectives.’
Retinas are complicated environments, and a breakdown of their natural working behaviour can happen in a number of different ways. Consequently, although all commercial implants aim to combat the failure of the natural vision-gathering cells and networks, they go about this task in two distinct approaches, termed subretinal and epiretinal variants.
Subretinal implants require a greater degree of surgical intervention, being inserted between the retina’s layer of sensory photoreceptors and the nourishing pigmented cell layer behind it.
Epiretinal implants are positioned on the inner surface of the retina itself, directly stimulating the retinal ganglion cells that transmit image information to different destinations in the brain. The epiretinal approach has the additional benefit of keeping most of the intrusive electronics off the retina itself, allowing the heat generated to be dissipated in the eye’s naturally humour-filled cavity.
Second Sight’s Argus II is an epiretinal implant – the only appropriate solution, according to Cosendai, and one which the company has also already used to successfully tackle retinitis pigmentosa (RP) using the same approach.
‘In AMD the retina is significantly more fragile than with RP, and epiretinal is the only solution,’ said Cosendai. ‘A subretinal implant would involve creating a retinal detachment and make the surgery unacceptably complicated, long and risky.’
According to the company, epiretinal implants are more long-lasting, with a lifetime of three years as well as a low rate of failure after a decade. Subretinal implants fare worse on both criteria, Second Sight said.
For all the advanced science behind the implant, the actual vision capture in the Argus II is accomplished by a standard image sensor very similar to ones now commonplace in mobile phones - although the subsequent data processing has required careful attention.
‘The video information is sent to a small computer who codes the grey levels in electrical currents,’ said Cosendai. ‘This coding is already pretty complicated, and it will become more complex as we better understand how the retina responds to electrical currents.’
In addition, the implant can deliver fine control over the stimulation delivered to the ganglion cells, allowing suitable levels of stimulation to be determined for each individual patient. The recuperation process includes time assessing how different currents elicit changes in visual perception, a process Second Sight refers to as ‘fitting’.
Argus II does its job by stimulating the retina, meaning it may prove unable to tackle scenarios where the retina is too damaged or if the connections behind the retina to the optic nerve and the brain have failed. But, Second Sight believes it will soon be able to demonstrate clinical progress there too, via a system called Orion.
‘There are a very large number of people who suffer from sight loss due to diseases that affect the optic nerve,’ Cosendai commented. ‘Orion is designed to send information directly to the brain, allowing those patients to have some level of vision back. We are making excellent progress to make Orion available soon, allowing us to potentially help 40 million people around the world.’